Targeted interventions by private and public sector are redefining healthcare
Published on November 30, 2022
By Aravindan Srinivasan, CEO, AVPN India Foundation & Director, Thematic Collaboration, AVPN and Dr. Neeraj Agarwal, Senior Director, CPHC System and Chief of Party, NISHTHA at Jhpiego

While Covid-19 has brought healthcare structures, and their resilience to the policy forefront, there is a parallel demand side conversation that needs to be undertaken. Broadly speaking, healthcare can be divided into preventive and remedial care. Starting from a simplistic model of health economics, one can argue that for most individuals, their net “level of health” or wellbeing hereafter, will be a cumulative of investments in preventive and remedial care. Rule of thumb would also suggest that preventive and remedial care would be trade-offs, investment in one, would either prevent or be at the cost of another. There are of course exceptions to this but for a simplistic generalization, this argument would hold.
The work of Pascaline Dupas on ‘Health Behavior in Developing Countries’ works in the similar field and brings out several insights critical and relevant to the Indian context. Further, given the disparity highlighted by the SDG index, we can contextualize the argument to the Northeast, and central India, the laggards in access and quality to healthcare, and try to elaborate on policy solutions that may be undertaken to bridge the lacunae.
The first insight from Dupas’ work is that access to health is intrinsically linked to access to knowledge, and by extension education. This insight may seem commonplace but is a powerful one. The healthcare issues identified by NITI Aayog for the Northeast SDG index are a case in consideration. – Continuing burden of HIV and other infectious diseases, Emerging challenges such as non-communicable diseases and Renewed focus on mental health issues.
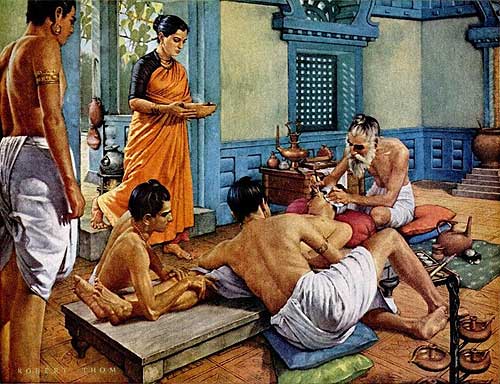
HIV, Tuberculosis, Diabetes, Heart ailments etc., are to large extent, manageable by behavioral and life-style changes. The same applies to policy objectives of maternal health, child nutrition and family planning. The key determinant here is the trade-off between preventive and curative health. Citizens need to be engaged and trained to prevent habits that lead to these diseases, look for signs for early diagnosis and educate on the cure available.
Second, is the role of the market, especially credit constraints, which impacts people’s ability to invest in health. Given the poor economic conditions of the masses in India, in most cases the choice is between food and essential utilities, and preventive health. This means (coupled with limited knowledge), the diagnosis is often delayed to a stage where cure is difficult and expensive. This is an essential limitation in the northeast – where financial challenges are coupled with topographical limitations. Usually access to primary healthcare is cumbersome and expensive- requiring high Out of pocket expenditure and taking leaves from work.
However, as Covid-19 has shown us, people are not always rational. Not everyone will invest in preventive care, even if they understand its impact on reducing risk of illness. This is also because humans make decisions based on short term needs. Here the role of behavior changes nudges, and price subsidies comes in. There have been several controlled trials proving the efficacy of Regular Camps and Incentives towards improving immunization rates in India. This similar model can be used to address the challenges in the Northeast. A simple “HealthCare Sunday” where local health and wellness center officials, come to the community to undertake health-checkups, engage on best practices, and incentivize healthy behaviors – such as handwashing, intake of folic acid, or use of condoms, through social and tangible incentives can go a long way in routinizing healthy behaviors.
According to a recent study, at least 70% and as much as 90% of the cardiometabolic risks are directly attributed to modifiable behaviors, hence, must be prevented through lifestyle changes. Evidence have shown that interventions aimed at behavioral risk factors and lifestyle changes could significantly prevent premature death worldwide with or without preventive medications and supplements. Moreover, most public health interventions are cost-effective making an integrated approach to health care may be a better option to reduce disease burden.
India’s goal for comprehensive care can be achieved only with simultaneous focus on preventive and curative care. For this, education, financial inclusion, and behavioral change are necessary. Until now, preventive care has been weak because of low incentive and focus on the issue from the public sector and for health care workers. On the contrary, the private sector has made significant progress towards preventive health checkups and overall wellness. This however has been limited largely to the financially stable sections of the market.
The private and public sector can thus intersect and collaborate on these capacities. The framework for “Complete and Comprehensive Care” already exists under the National Health Policy that can be expanded upon to include preventive care. The scale and long-term impact of can further India’s goal of healthcare for all, while emerging as a global leader in line with India’s historic ethos of harmony of mind, body, and spirit. ENDS